Protein Capsule Bacteria
To search the entire book, enter a term or phrase in the form below
Custom Search
Bacterial Defense against Phagocytosis
© Kenneth Todar, PhD
Introduction
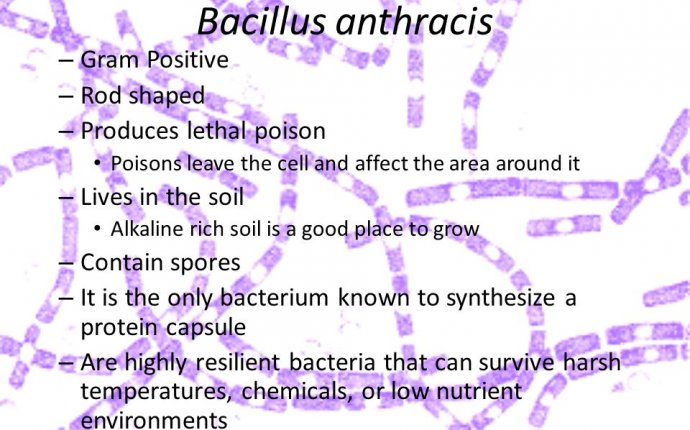
Some pathogenic bacteria are inherently able to resist the bactericidal components of host tissues, usually as a function of some structural property. For example, the poly-D-glutamate capsule of Bacillus anthracis protects the organisms against action of cationic proteins (defensins) in sera or in phagocytes. The outer membrane of Gram-negative bacteria is a permeability barrier to lysozyme and is not easily penetrated by hydrophobic compounds such as bile salts in the GI tract that are harmful to the bacteria. Pathogenic mycobacteria have a waxy cell wall that resists attack or digestion by most tissue bactericides. And intact lipopolysaccharides (LPS) of Gram-negative pathogens may protect the cells from complement-mediated lysis or the action of lysozyme.
Most successful pathogens, however, possess additional structural or biochemical features that allow them to resist the host cellular defense against them, i.e., the phagocytic and immune responses. If a pathogen breaches the host's surface defenses, it must then overcome the host's phagocytic response to succeed in an infection.
Ability of Pathogens to Avoid or Overcome PhagocytesMicroorganisms invading tissues are first and foremost exposed to phagocytes. Bacteria that readily attract phagocytes and that are easily ingested and killed are generally unsuccessful as pathogens. In contrast, most bacteria that are successful as pathogens interfere to some extent with the activities of phagocytes or in some way avoid their attention.
Bacterial pathogens have devised numerous and diverse strategies to avoid phagocytic engulfment and killing. Most are aimed at blocking one or more of the steps in phagocytosis, thereby halting the process. The process of phagocytosis is discussed in the chapter on Innate Immunity against bacterial pathogens.
Avoiding Contact with Phagocytes
Bacteria can avoid the attention of phagocytes in a number of ways.
1. Pathogens may invade or remain confined in regions inaccessible to phagocytes. Certain internal tissues (e.g. the lumens of glands, the urinary bladder) and surface tissues (e.g. unbroken skin) are not patrolled by phagocytes.
2. Some pathogens are able to avoid provoking an overwhelming inflammatory response. Without inflammation the host is unable to focus the phagocytic defenses.
3. Some bacteria or their products inhibit phagocyte chemotaxis. For example, Streptococcal streptolysin (which also kills phagocytes) suppresses neutrophil chemotaxis, even in very low concentrations. Fractions of Mycobacterium tuberculosis are known to inhibit leukocyte migration. The Clostridium ø toxin also inhibits neutrophil chemotaxis.
4. Some pathogens can cover the surface of the bacterial cell with a component which is seen as "self" by the host phagocytes and immune system. Such a strategy hides the antigenic surface of the bacterial cell. Phagocytes cannot recognize bacteria upon contact and the possibility of opsonization by antibodies to enhance phagocytosis is minimized. For example, pathogenic Staphylococcus aureus produces cell-bound coagulase and clumping factor which clots fibrin on the bacterial surface. Treponema pallidum, the agent of syphilis, binds fibronectin to its surface. Group A streptococci are able to synthesize a capsule composed of hyaluronic acid. Hyaluronic acid is the ground substance (tissue cement) in connective tissue. Some pathogens have or can deposit sialic acid residues on their surfaces which prevents opsonization by complement components and impedes recognition by phagocytes.
Inhibition of Phagocytic Engulfment
Some bacteria employ strategies to avoid engulfment (ingestion) if phagocytes do make contact with them. Many important pathogenic bacteria bear on their surfaces substances that inhibit phagocytic adsorption or engulfment. Clearly it is the bacterial surface that matters. Resistance to phagocytic ingestion is usually due to a component of the bacterial cell surface (cell wall, or fimbriae, or a capsule). Classical examples of antiphagocytic substances on bacterial surfaces include:
1. Polysaccharide capsules of S. pneumoniae, Haemophilus influenzae, Treponema pallidum and Klebsiella pneumoniae
2. M protein and fimbriae of Group A streptococci
3. Surface slime (polysaccharide) produced as a biofilm by Pseudomonas aeruginosa
4. O polysaccharide associated with LPS of E. coli
5. K antigen (acidic polysaccharides) of E. coli or the analogous Vi antigen of Salmonella typhi



